Supporting Those Who’ve Lost Loved Ones: A Day in the Life of Willis Partington
Welcome to “A Day in the Life”—the Frontline series that follows team members from different parts of VNS Health as they go about a typical day fulfilling our organization’s mission—to improve the health and well-being of people in the home and in the community.

Today, we feature a day in the life of… Willis Partington, Lead Bereavement Counselor for VNS Health’s hospice program. Besides supervising the bereavement team and providing solace, and a listening ear to bereaved family members and caregivers, he also offers support to members of the hospice team—and beyond. We asked Willis to take us through a typical day.
6:30 a.m.

I wake up at 6:30, which is when things start happening around the house; my wife is getting ready for work and waking up my son, who’s in high school. At around 7:00, I’ll have my morning coffee and juice and a breakfast of scrambled eggs on toast with avocado. It’s a delicious, healthy, filling way to start the day!
8:20 a.m.
I pop open my laptop and check emails to see whether any deaths happened overnight, or if there’s any other issue I might have missed the previous day that I need to follow up on. I also log on to our clinical support platform, HomeCare HomeBase, to check on any new patient deaths or other reports in the areas I cover, which are Manhattan’s Upper and Lower West Side, This way, I have the most updated information and am prepared for my first meeting of the day.
Although I have my share of scheduled meetings, as a bereavement counselor a lot also happens in my day that’s unscheduled—much like death itself.
9:00 a.m.

We do weekly morning Zoom meetings with the whole hospice team in which we discuss half the patients under our care, based on patients’ last names. One week might be A through K, the next week L through Z. The first order of business of the team meeting would be any general announcements. Then the hospice team manager will turn it over to me and we’ll review the deaths of the patients who’ve passed away over the last seven days.
At that point, I’ve already gone into the patients’ charts in HomeCare HomeBase and I’ll have a sense of who the primary caregiver and the primary bereaved are in the family; they might be one and the same, but often they’re not. An adult daughter, for instance, might have been the main point person and caregiver, but an elderly spouse might be the one most in need of support after the death. I’ll also know who was on that patient’s hospice team—be it the nurse, spiritual-care counselor, social worker, or anyone else. I always get a lot of valuable information from the team about the circumstances around the death and how the family is coping, all of which helps me when I reach out and make that first phone call to offer bereavement services.

Bereavement services are unique in that they’re optional. Often, I’ll reach out to a family and they’ll say thanks but no thanks, we’re fine and really aren’t interested. Some just want a call or two. Other times I’ll make a call and the person will start crying and talking the minute I introduce myself. Sometimes people will go on to take advantage of every support group and service we offer.
I often say that we spend 15% of our time with 85% of grieving family members, and 85% of our time with 15% of our bereaved families.
10:00 a.m.
On Tuesdays, I’ll send out an email to ask for RSVPs for our weekly Tuesday evening bereavement Zoom group. This is the largest group we offer, and one of several drop-in groups we have. Before the pandemic, this was a much smaller, in-person gathering, drawing maybe a dozen people. But demand surged during the pandemic, which made bereavement issues even more challenging due to the forced loneliness and isolation. So now it’s a Zoom meeting, primarily for bereaved family members from our VNS Health Hospice, but anyone who’s experienced a loss can join.
1:00 p.m.

Lunchtime for me is usually a smoothie, something I’ve gotten into lately. I do a combination of different fruits and kale with some yogurt.
3:00 p.m.
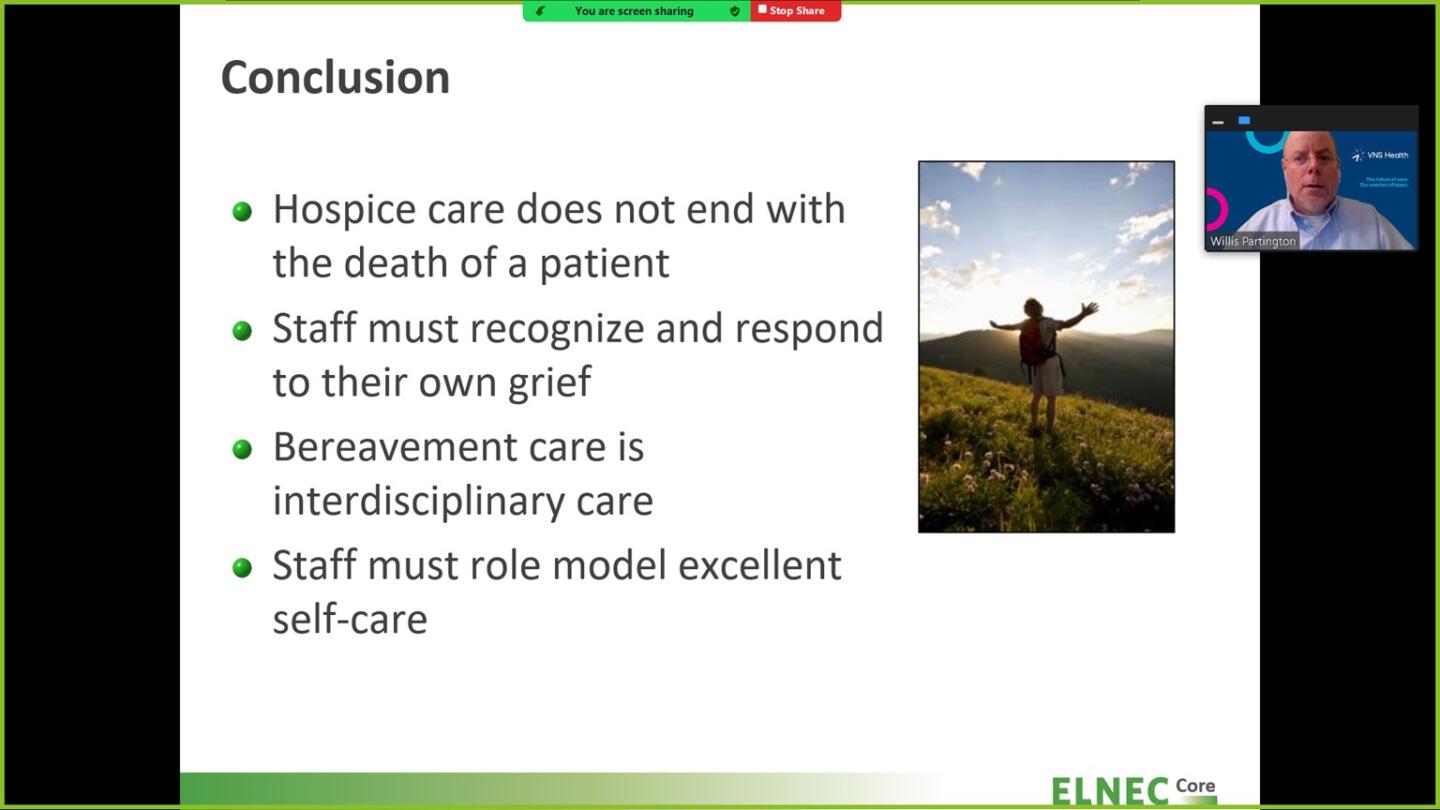
As part of my job, I lead a bereavement and/or ethics orientation for new employees, who might be hospice team members or even employees from other parts of the organization. This is basically an overview of our bereavement program and about what working with grief and loss entails. Everybody who works in hospice works with grief and loss by definition, of course, but sometimes employees are dealing with loss in their personal lives as well. A good portion of this meeting is dedicated to emphasizing the importance of self-care, which is critical in terms of having the sustainability to do this kind of work.
6:00 p.m. – 7:30 p.m.

On Monday evenings, I lead a men’s bereavement Zoom group, Men Coping with Grief. Tuesday evenings is when we host For Adults Grieving the Death of a Loved One, the ongoing drop-in group I mentioned earlier. At this point, I’ll have received my RSVPs and will have a sense of how many people we need to plan for. Because the groups are larger now, I have another facilitator join me Zoom, and we randomly assign participants to our two breakout rooms. After the meeting, my colleague and I talk about how things went in our breakout rooms. Maybe a topic was raised that will prompt me to send out an article, poem, or quote to the group that might relate to that theme. Tuesdays are my late nights—I might not have dinner until 9:00 p.m.!
More from Willis Partington, Lead Bereavement Counselor, VNS Health Hospice Care
When we’re providing bereavement counseling, we try to talk to people on a bi-weekly or monthly basis, because talking every week can create a dynamic in which it may start to feel like therapy. Our role is to walk a grief journey with people, to provide them with information, education, and normalization. It’s about counseling—not therapy. When people are doing the work of grief and mourning, my work with them is energizing and deeply rewarding.

The support we offer can take many forms. For an elderly person who’s suddenly alone after a spouse of 60 years has died, isolation and loneliness are a primary concern. Small things like listening to classical music, getting a pet to care for, or leaving a light on so you don’t come back to a dark apartment, can offer some comfort—simple as these may sound.
Some people—especially those who spent years as full-time caregivers for their loved ones—suddenly feel like they have no purpose in life, particularly if they’ve given up jobs or activities in the process. They may be confused as to their new identity. So maybe for them it’s about identifying the few things that they might not have given up, so they can grasp onto those as they rebuild their own life.

Many people are reluctant to consider support groups because they think they’ll be depressing, and they’re surprised when I tell them that those sessions contain laughter much more than tears. Sometimes it’s just about reassuring someone that they’re not crazy or acting irrationally, which is a common concern. It’s perfectly okay to talk to a framed photo of your deceased spouse if it brings you comfort, or to announce, “I’m home” when you return to an empty house. We also do a partnership with MoMA in which grieving family members go to the museum and get in-depth talks from experts about the art—nothing at all to do with death or bereavement. And those group outings can be wonderful as well.
I would sum up what we do this way: Members of the hospice team walk the family on a journey from life to death, while the bereavement team walks with them on a journey from death to new life.


