Objectives in Action:
“No Medicaid? No Problem!”
Welcome to our new series, “Objectives in Action.” Each month, we’ll feature a team from across the organization that’s working to make one of our 4 Top Company Objectives a reality. First up, our Health Plans’ Medicaid Operations team.

Top Company Objective: Lead New York State in integrated long-term care (MAP)
Team: Medicaid Operations
The situation: About one-third of the people who apply to our two Medicaid long-term care plans—Managed Long Term Care (MLTC) and Total (our Medicaid Advantage Plus, or MAP plan)—have errors or lapses in their Medicaid coverage that need to be fixed before they can enroll.
As if that isn’t challenging enough: Processing the paperwork and getting state approval to enroll someone into a plan was taking a long time—79 days on average.
Top Company Objective in action: To address these issues, the Medicaid Operations team, which is part of the Health Plans’ Medicaid Eligibility Unit (MEU) and consists of 9 team members, took the following steps to Simplify and Empower their handling of Medicaid applications:
- The Medicaid Operations team started using upgraded technology so that referrals can be sent directly into the team’s database through our new Health Plan Provider Portal.
- The team has also been submitting prospective member applications electronically to New York State, so applications are getting processed faster.
- In addition, the reporting system for Medicaid-pending cases was revamped to focus on the applications that need the most support.
The results: With these changes, the team has cut in half the time it takes to fix Medicaid issues and get consumers enrolled in our MAP or MLTC plans. What used to take about three months now takes just six weeks.
Why it matters: Faster enrollment into our Medicaid plans means more Health Plan members are able to move right into integrated care plans such as our MAP plan—perfectly in support of our Top Company Objective.
Driving toward our 3-year Strategic Goals: Increasing membership in our MLTC and MAP health plans contributes to our goal of having 100,000 patients, members and clients in our care by 2026. The changes that the Medicaid Operations team have implemented will also help us achieve our 3-year Strategic Goal of providing 5-Star Quality and Consumer Experience across the organization.
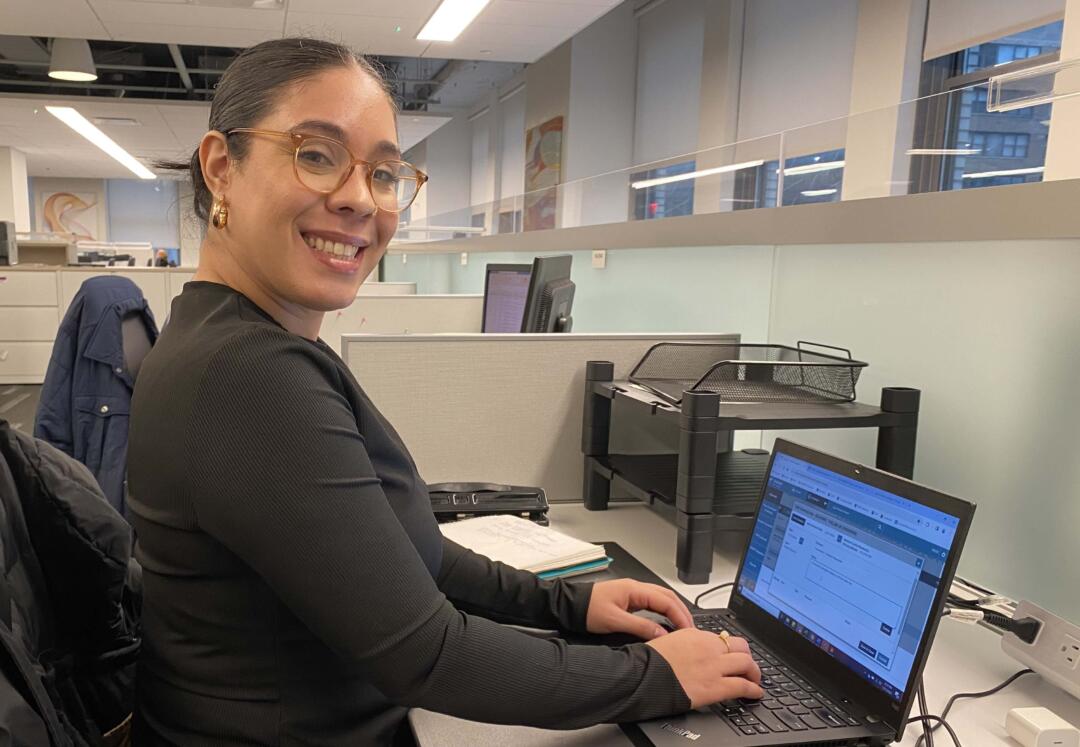
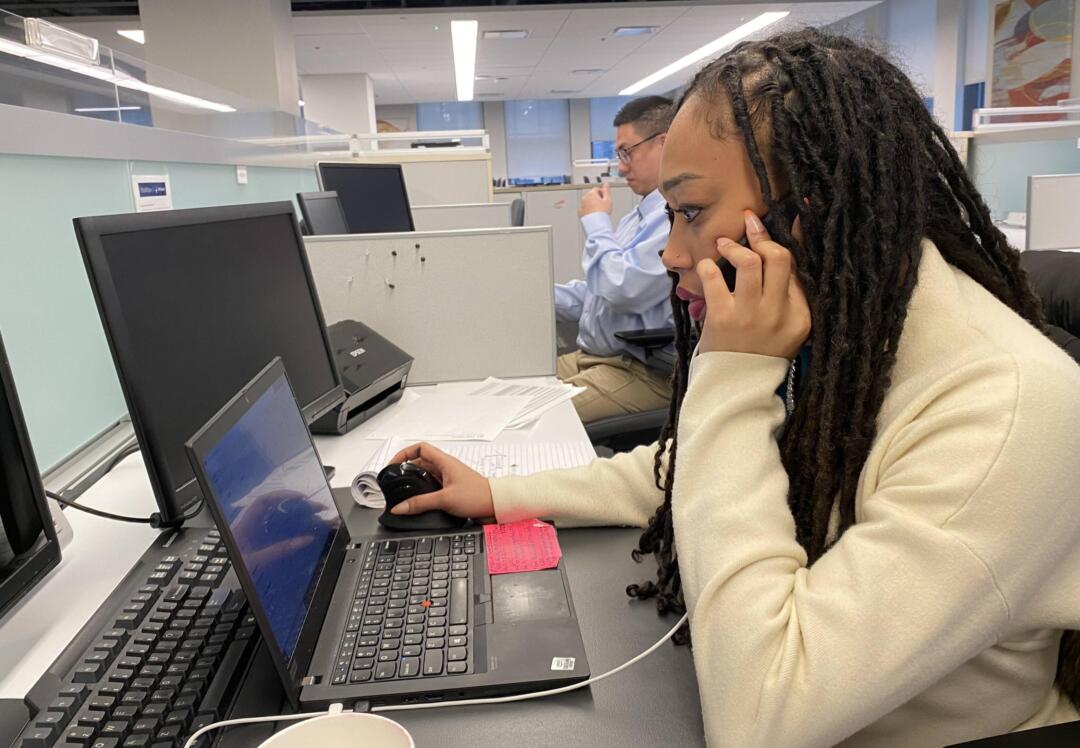
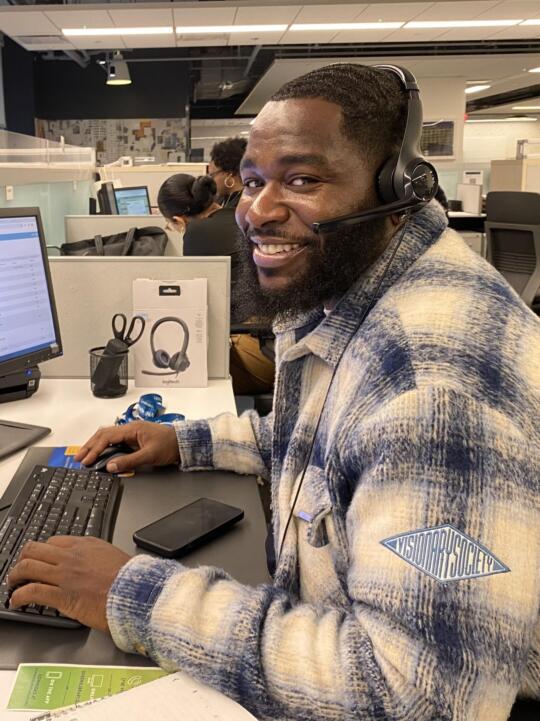
What the Medicaid Operations team members are saying: “If someone has an issue that’s keeping them from being eligible for Medicaid long-term care, the Medicaid Operations team makes the necessary corrections,” says Amanda Zaragoza, Manager, Medicaid Operations. “We call the state Medicaid office to see what’s needed, then we fill out the documents and submit them. The potential MLTC or MAP member just has to sign the forms—we do the rest.” Or as Paul Staley, one of the team’s Medicaid Eligibility Coordinators, puts it: “No Medicaid? No problem!”
To view a video of MEU team members discussing the changes they’ve put in place, click on the video image here below.
For more on VNS Health’s 3-Year Strategic Plan, click here.