VNSNY’s New CMO Takes Home Care to the Next Level
Aimed at Reducing ER and Hospital Visits for High-Risk Populations, VNSNY Launches Care Management Organization
 VNSNY has added a new business unit—a Care Management Organization (CMO) that will work with insurers to provide their high-risk members with enhanced care management services in a home-based setting. Following approval from the New York State Department of Health, the new unit officially launched on May 6th.
VNSNY has added a new business unit—a Care Management Organization (CMO) that will work with insurers to provide their high-risk members with enhanced care management services in a home-based setting. Following approval from the New York State Department of Health, the new unit officially launched on May 6th.
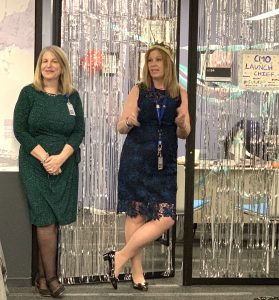
At the roll-out of VNSNY’s new Care Management Organization (CMO) on May 6th, EVP and Chief of Provider Services Andria Castellanos (left) and SVP for Population Health Rose Madden-Baer congratulate the CMO staff on their hard work preparing for the launch.
“With this new CMO, we’re providing insurers what they need most—a cost-effective way of keeping their high-risk plan members out of the ER and the hospital,” says Rose Madden-Baer, VNSNY’s Senior Vice President for Population Health and Clinical Support Services. The CMO is currently contracted with VNSNY CHOICE Health Plans to manage members of its two integrated Medicare-Medicaid plans, CHOICE Total and CHOICE FIDA Complete. “We’re actively exploring arrangements with other integrated Medicare-Medicaid plans in our service area as well,” adds Rose.
To be eligible for the CMO, plan members must be identified as having at least seven common co-morbidities, such as congestive heart failure, COPD, diabetes and hypertension—a profile that VNSNY’s Analytics team has found to be a good evidence-based measure of increased risk. Those found to qualify will be followed by the CMO team for 12 months and then reevaluated. In addition, the CMO will target a smaller group of members to receive post-acute care management for a period of 60 days following discharge from the hospital.
 Both groups will have access to a wide range of CMO services, including an initial assessment by a visiting nurse, ongoing support services such as medication reviews, telephone check-ins and “virtual visits” as well as remote monitoring, referrals for other community-based supportive resources, behavioral health and other in-home skilled services as needed, and home visits by a nurse practitioner if an urgent health issue arises. Members suffering from advanced disease processes may also be referred to the CMO’s Advanced Illness Management (AIM) program.
Both groups will have access to a wide range of CMO services, including an initial assessment by a visiting nurse, ongoing support services such as medication reviews, telephone check-ins and “virtual visits” as well as remote monitoring, referrals for other community-based supportive resources, behavioral health and other in-home skilled services as needed, and home visits by a nurse practitioner if an urgent health issue arises. Members suffering from advanced disease processes may also be referred to the CMO’s Advanced Illness Management (AIM) program.
“The CMO integrates all the different population health capabilities that VNSNY has been developing over the past several years, including advanced patient monitoring, real-time alerts when health problems arise, and enhanced performance measurements,” says Rose. “We’re essentially taking home care to the next level by pooling all of our expertise to offer extended, home-based care management services for our most vulnerable patients.”
To read about how our CMO has already helped two vulnerable CHOICE members, click here.

