Five Years Ago, Our Lives Changed. Team Members Look Back on the COVID Pandemic.
Five years ago this month, the COVID-19 virus hit New York with a fury, causing a dramatic change to everyone’s lives.

As the number of infections began mounting, VNS Health rose to the challenge: Beginning this week of March, 2020, all of our teams swiftly pivoted to address the pandemic.
In this Frontline special feature, VNS Health team members reflect on what they and their teams were doing five years ago to help our organization address the challenges of COVID, so we could continue to support vulnerable New Yorkers—and each other—during the largest pandemic in modern history. As you’ll see, our three Core Values of Empathy, Agility and Integrity played a key role in all that we did.

“Something to really be proud of.”
“When COVID hit in early 2020, Marki Flannery was CEO and I was Chief Financial Officer. What we were going through in New York at that time was unique—we were losing team members, and a lot of our team members were losing family members. As I look back, the agility this organization showed in the face of those very scary times was truly incredible. Entire programs that had been in person became remote very quickly, and we were still able to deliver in important ways on behalf of our mission that was set 130 years ago.
How we came out of that—ensuring financial stability so that we could keep as many people employed as possible and continue doing the things we do for our mission—was truly amazing. This organization has weathered so many storms over the course of a century and a quarter, including COVID, and we are still here, serving more New Yorkers than we’ve ever served, in more geographies than we’ve ever served before. That’s something to really be proud of.”
—Dan Savitt, President and CEO

“Practically overnight, we transitioned from in-person assistance to fully remote support.”

“At our 42nd Street office, the IT team reported to the office daily, ensuring employees had the computers, support, and tools they needed to work remotely. Practically overnight, we transitioned from in-person assistance to fully remote support—leveraging Teams, Zoom, and remote-access tools to troubleshoot issues from afar. Even hardware repairs adapted to this new reality, with employees mailing in their computers for servicing. Fortunately, the team was already in the midst of a scheduled computer upgrade, with a well-structured process and additional staff in place to handle the workload efficiently.
Beyond maintaining business continuity, the team played a crucial role in setting up a vaccine clinic. The team set up 15 small stations, ensuring computers were well connected to enable seamless data tracking. I remember working 28 days straight in the clinic, making sure IT issues never became a barrier. I didn’t want anyone left behind because of a technical problem.”
—Sunny Babbar, Manager, IT Support

“We dramatically changed the way we worked.”

“Overnight, we dramatically changed the way we worked. People went remote, and we added tools and technology to communicate, collaborate and monitor productivity. We learned a lot and we applied that learning, designing a work model that we still have today—flexible enough so people can work at home but stay connected through technology.”
—Andrea Spencer, Director, Care Management Organization (CMO)

“We had to be tremendously agile.”

“We set up the CERT (Clinical Expertise Response Team) phone line to screen field employees for COVID symptoms and answer their questions on protocols, PPE use and potential exposures. We had to be tremendously agile to set it up so quickly in partnership with the call center. CERT ended up handling almost 9,000 inquiries from field clinicians and HHAs in 2020. We were working around the clock, providing information and support, and listening to team members’ experiences and challenges in the field—going that extra mile for our employees and our patients.”
—Catherine Schaefer, Vice President, Quality and Performance Improvement

“That’s what you’re there for—you’re a nurse, that’s your profession and your responsibility.”
“The main thing was working through fear of the unknown. We followed strict protocols, including donning PPE and scheduling COVID-positive patients at the end of the day. You just have to trust in your training, your knowledge and your practice. That’s what you’re there for—you’re a nurse, that’s your profession and your responsibility.”
—Gregory Fargas, RN, Brooklyn Home Care

“We listened to their questions and fears: ‘I’m scared, what do I do?'”

“When the pandemic hit, one important thing I and my colleagues did was help our home health aides get their questions answered and get what they needed. We listened to their questions and their fears: ‘I’m scared, what do I do?’ ‘My patient needs this, how do I get it?’ I made sure whoever needed information got that information, and that whoever needed supplies got those supplies. People would say, ‘Call Rosa, she’ll get it.’ It was a very rewarding feeling.
With Amanda Weiner [Director, Organizational Effectiveness, Learning and Development], we also set up regular HHA support calls—with upwards of 300 HHAs on each call—to help them navigate technology, PPE and rapidly changing protocols, and to get their questions answered and fears addressed. Although less frequent now, the support calls continue to this very day.”
—Rosa Marcus, Director, Support Services, Personal Care

“We held daily huddles each morning and each afternoon.”

“Our Clinical Education team was committed to doing our part—to orient our clinicians to home care, and equip them with the knowledge they needed to go out and take care of patients in the midst of the pandemic. We held daily huddles each morning and each afternoon, and we also checked on each other throughout the day, reassuring team members and making sure everybody was together, connected and okay. It was a new level of camaraderie.”
—Elizer Cooper-Audain, Associate Vice President, Education & Development

“Even though we weren’t all in the same place, we were connected.”
“Going through a crisis like that wears on you, but it also strengthens you—as an individual, a team, and an organization. I never felt alone. Even though we weren’t all in the same place, we were connected. Every day there was an obstacle—and innovative thinking to solve it. Everyone could see just how committed VNS Health was to New Yorkers, to serving our patients.”
—Sandy Merlino, Vice President, Business Development

One of the ways we all stayed connected – and stayed inspired – was through daily CEO audio messages. You can listen to some of them by clicking here.

“We all drew on something bigger than us.”

“We all drew on something bigger than us. We knew the organization had a legacy of springing into action to address public health needs of the community at a time of crisis. We had a duty to our hospital partners—who were in crisis themselves—to help transition patients home in order to care for more people. It has always been our central purpose, for over 130 years, to be a glue holding things together in the New York healthcare ecosystem.
Initially, the lack of personal protective equipment (PPE) was one of the most crucial gaps we had to fill. I spent a large part of my time in those first few weeks advocating for access to PPE with our elected officials, associations, government partners, and whatever other channels we could. We were in a particularly tough spot because we came after hospitals in the pecking order—but in order to help them discharge patients into the home and free up beds, we needed PPE to protect our own employees. It required a lot of leadership and advocacy on our part.
Once we got the PPE, we had to create safety protocols for donning and doffing in an urban home-based setting, because no protocols for this existed. We went on to share those protocols with home care organizations around the country who experienced the peak of the pandemic after we did.
We were also committed to getting surgical masks into the hands of our HHAs, who were spending hours in patients’ homes. The fastest way to do that was to manually mail thousands of packets of surgical masks out to our 6,000 home health aides. It was a meaningful experience for everyone involved.”
—David Rosales, EVP, Chief of Provider Services

“It was my Lillian Wald moment.”

“I was working remotely when I learned they needed volunteers to create PPE COVID kits. I said, ‘I’ll do it.’ I called my mother, who was a factory worker, to pick her brain about creating an assembly line. I also found an OSHA course online about PPE and took that after work. Later, I helped set up our vaccine clinic. I learned so much from everyone around me, about lot numbers, temperature control, cross-contamination. I learned more in the two years of the pandemic than at any other time. It was the hardest, scariest, most profound event of my career. It was my Lillian Wald moment.”
—Diana Vargas, Procurement Associate

“We really appreciated what our frontline team members were going through and did whatever we could to support them.”
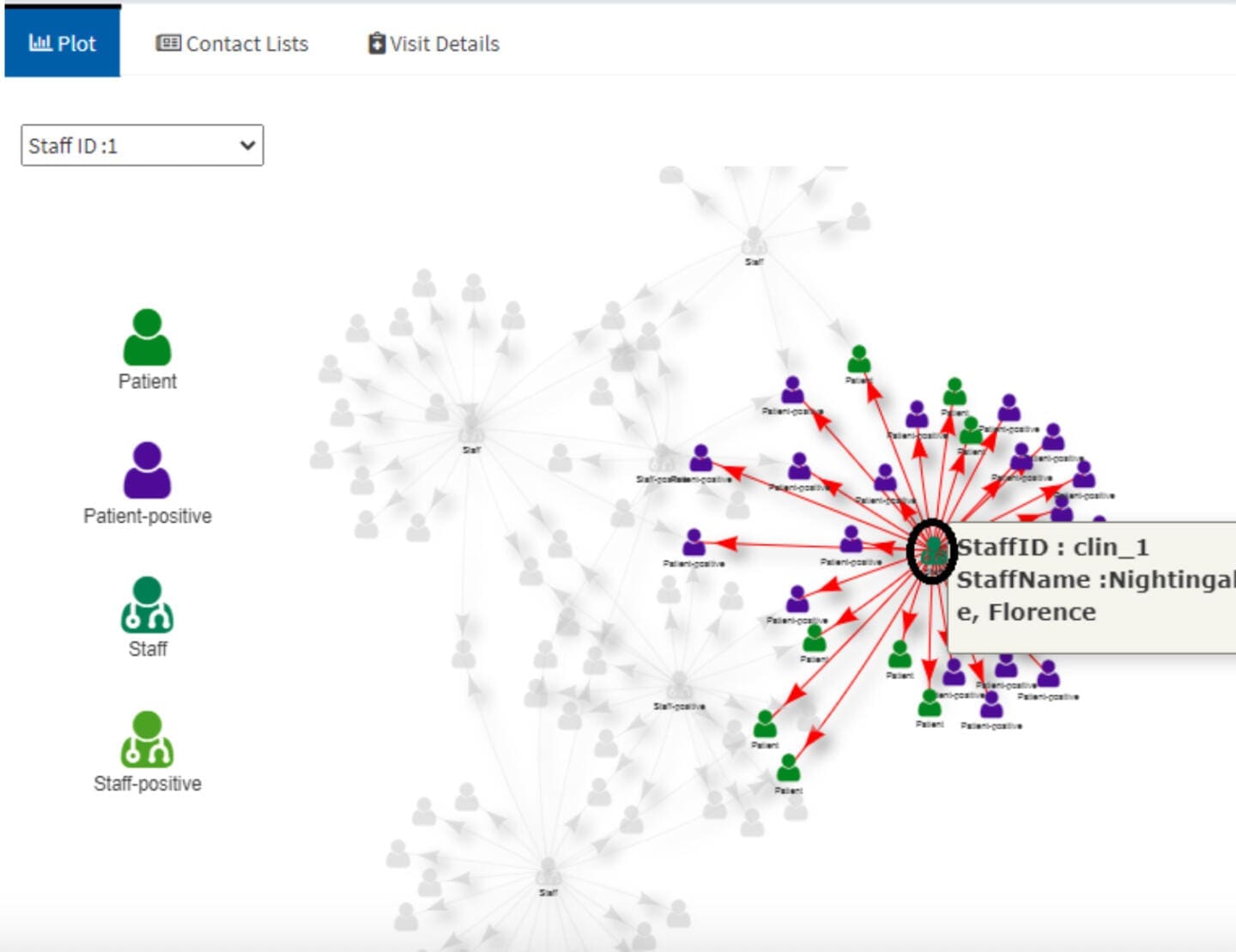
“Technologically, our team was well prepared to work remotely, but psychologically we weren’t. We tried to connect as much as we could. It was a big shift in our priorities. How do we support the organization, what information do they need? We really appreciated what our frontline clinicians were going through and did whatever we could to support them. We built an application that created trees of exposure to help us contact trace among our patients and clinicians. If we found a patient had COVID and we had a date, we could see who visited them, see who that clinician visited—and notify people of potential exposure. We also released the contact tracing app so other home care agencies could use it.”
—Tim Peng, Chief Analytic Officer, Head of Business Intelligence & Analytics

“Our focus stayed exactly the same as ever, helping people have a comfortable death.”

“There is a lasting camaraderie among everyone in health care who went through COVID. We all went together into the unknown, the best we could. The biggest challenge for our hospice teams was that families couldn’t be there. It was a very different type of death. It was so sudden, it didn’t allow patients and their families any end-of-life process. A lot of these patients were awake and alert and knew they’d never see their family again. Thank goodness for technology, which at least allowed them to hear their loved ones’ voices. Still, there’s no substitute for the real thing. At the same time, our focus stayed exactly the same as ever, helping people have a comfortable death.”
—Diane Lynch, Hospice Liaison

“The first thing we did was call more than 10,000 members of the Chinatown Community Center.”

“When COVID hit, we were concerned about live-alone seniors being isolated at home. The first thing we did was call more than 10,000 members of the Chinatown Community Center to make sure they were okay, and that they had what they needed at home—PPE, food, information, and resources. Those who could, we taught to use Zoom so they could connect with our programming, including health education and music concerts. In crisis, we draw people together to help our seniors live better in the community.”
—Carrie Ng, Manager, VNS Health Community Centers

“VNS Health did not close. We kept going—we were on top of it.”

“During the pandemic, folks with mental health struggles were left out there with a lack of access to care. Hospitals closed certain services and schools closed, but VNS Health did not close. We kept going—we were on top of it. From the beginning, we did a lot of telehealth. That’s how we connected before we got official platforms up and running. The pandemic also raised awareness of mental illness and our programs and funding got extended, so something good came out of it.”
—Debra Thomas, Associate Director, Crisis and Assessment, Behavioral Health

“I knew how to care for my patients safely.”

“I got COVID in 2020, and I was suffering so much—headache, fever, weakness, trouble breathing. My family was so scared. I isolated in one room, and I prayed. When I got better, I said, ‘I’m going to help people with COVID.’ I understood how they were feeling—when you’re in bed and suffering alone, it’s so sad and scary. So I went back to work. I knew how to care for my patients safely: You just have to make sure that you take care of your PPE, and take care of yourself.”
—Arcina Batista, Home Health Aide, Personal Care

“We created a task force and a dashboard to keep track of members who were sick, hospitalized, recovered, or succumbed.”

“A lot of folks were anxious, so we had to call all our members. And we had to come up with a way to stratify members to determine who’s at risk right now, who really doesn’t have a backup plan in place, who needs personal care in their home. Managing the spread, the masks, the transportation—we had to manage it all. We created a task force and a dashboard to keep track of members who were sick, hospitalized, recovered, or succumbed. Collaboration and coordination helped us through. We worked closely with our partners on telehealth assessments, on getting meals to our members’ doors, and on providing the continuum of care to get through this crisis.”
—Esther Conteh, Vice President, Care Management, Health Plans

“I felt so fortunate to be part of the VNS Health workplace family.”

“It was a scary, uncertain time five years ago. I felt so fortunate to be part of the VNS Health workplace family that fostered such a strong sense of duty, purpose and belonging. I felt it was particularly important to support our members. They had lots of concerns and questions, so I encouraged an especially open line of communication and was vigilant about putting people in touch with the resources and programs that could help them. It’s amazing what the power of human connection can accomplish during a collective crisis like COVID.”
—Lidia Medina, Contact Center Agent, Contact Center Shared Services

“With the COVID vaccine, we finally felt like we had something, and I love that our organization played such a central role in distributing it.”
“With the COVID vaccine, we finally felt like we had something, and I love that our organization played such a central role in distributing it. Our in-house vaccine clinic effort was an incredible turning point. Then came the wave of vaccine mandates, and I became known as the vaccine mandate queen. There were so many layers of vaccine mandates—local, state, federal. It was changing constantly, and navigating that became my full-time job for several months.”
—Nausheen Rokerya, Vice President, Associate General Counsel

the COVID vaccine.

“Our vaccine clinic was a labor of love for everyone involved.”
“Our vaccine clinic was a thing we could do to give back to our team members for all the sacrifices that they were making, and to help keep our patients and members safe. We all helped in any way we could to vaccinate as many as we could and make sure we never wasted a dose. The clinic was a labor of love for everyone involved.”
—Annie Miyazaki-Grant, SVP, Chief Compliance & Privacy Officer

“There was so much great thinking and collaboration throughout the pandemic.”

“I think the vaccine clinic was our greatest accomplishment. It allowed us to come back to the office. My team did whatever was needed for people to come back—especially the maintenance staff, who came in every day and met by Zoom each day at 3 p.m. to go over everything, and were the front lines for our facilities. We installed sanitizers and wipes, making spaces ready for people to come back and distance appropriately. We put up plexiglass, which wasn’t easy to source in those early days, and we developed plans for social distancing. There was so much great thinking and collaboration throughout the pandemic. Everyone went the extra mile. I love what we do. I’m committed to helping our frontline do what they do so our mission gets delivered.”
—Jay Margolias, Vice President, Facilities and Property Management

Frontline Flashback: VNS Health Heroes of 2020
Team members from across the organization demonstrated incredible heroism throughout the pandemic. We profiled a number of these team members in Frontline at the time. To read these profiles and to see other COVID-related Frontline stories and videos, click here.


