Congratulations to Our Third Generation of Lean Six Sigma Green Belts!

VNS Health is now in its third year working with Lean Six Sigma—a set of management tools that help organizations to operate more efficiently and improve the quality of their services and products.
Building on the success of previous years, Tony Dawson, Chief Quality Officer for Provider Services, recently took a new group of 24 VNS Health team members through a six-month course that prepared them to be certified as Lean Six Sigma Green Belts. “Our latest cohort did a tremendous job,” Tony reported. “Besides gaining valuable skills in how to analyze tough problems and develop solutions, they also learned to negotiate, compromise and communicate with each other.”
For their final projects, course participants broke into five smaller groups to put their learnings into action as they tackled specific issues in VNS Health’s operations. To read summaries of these final projects along with the names of our newest Green Belts, click on the project titles below. As you’ll see, these team members had a real impact on some knotty problems!
LEAN SIX SIGMA 2022 FINAL PROJECTS (Click on each project to read more or scroll below.)
Personal Care: Improving Home Health Aide Compliance with Their Patients’ Plan of Care
Home Care: Developing a Tool to Help Reduce Hospitalization Risk
Home Care and Hospice Care: Standardizing the Monitoring and Treatment of Complex Wounds
Behavioral Health: Improving the Health Home Program’s Operations
Hospice Care: Reducing Hospitalizations of Hospice Patients
Special thanks to this cohort’s Lean Six Sigma Executive Sponsors and Coaches:
Executive Sponsors—Andria Castellanos, Jessica Fear, Rose Madden-Baer, Jennifer Brullo and James Rolla
Coaches—Kennya DiLegge, Deb O’Hehir, Catherine Schaefer, Erica Popp, Linda Smith, and Daniel Belloise, with thanks to Nadesia Biart for providing administrative support.

Personal Care: Improving Home Health Aide Compliance with Their Patients’ Plan of Care
Project Leads
- Shama Barrett, Manager, Bronx/Queens Certified Services, Personal Care
- Alexandra Duma, Associate Project Manager, Personal Care
- Wendy Mendoza, Account Manager, Business Development
- Lauren Campbell, Director, Emergency Response Systems, VNS Health Safety and Security
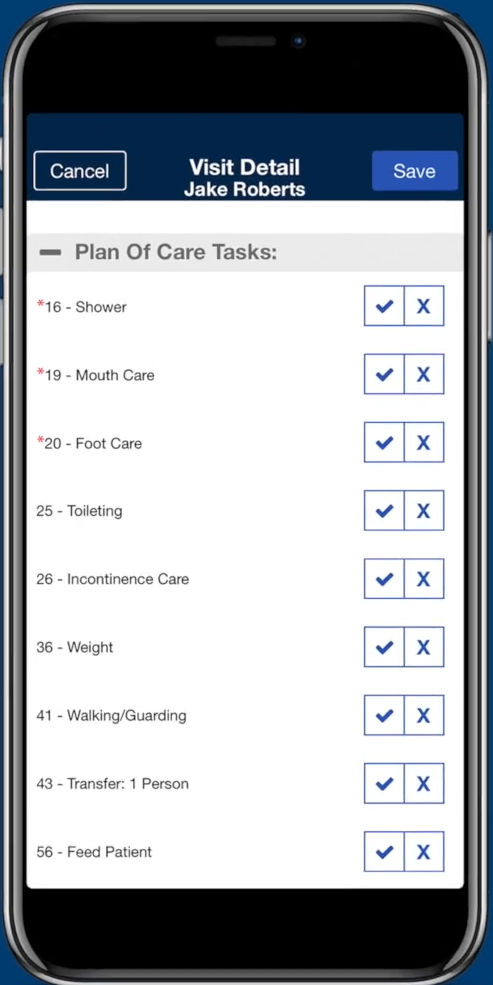
In this project, the team looked at ways to enhance the compliance rate of VNS Health’s home health aides (HHAs) in checking off completed tasks for their patients’ Plan of Care. The project team identified a number of ways to potentially enhance HHAs’ ability to access their plan checklists, including improving communication between the HomeCare HomeBase clinical care platform and the HHAx phone app, which lets HHAs complete and submit their Plan of Care digitally.
Following this, the project team conducted several pilot tests to see if a three-hour in-person training session improved HHAs’ adherence to the Plan of Care. In this training, 14 HHAs were coached on proper clock-out procedure. The team tracked the pilot group’s adherence to checking off the Plan of Care both before and after the training, and found that the training increased compliance rates from 58% to 70%.
The team also proposed changes to the HomeCare Home Base and HHAx systems to enable more efficient communication. These included providing HHAs with a more reliably up-to-date Plan of Care, and documenting compliance with the daily Plan of Care more effectively.

Home Care: Developing a Tool to Help Reduce Hospitalization Risk
Project Leads
- Allison Simms, Associate Director, Rehab Services, Queens Home Care
- Li-wen Tsai, Quality Improvement Manager, Clinical, Quality Care Management
- San Le, Director, Provider Intake & Credentialing, MSO
- Jason Tsui, Manager, Corporate Support Service Operations, Document Control Unit
- Robert Orlando, VP, Software Engineering and Product Development, Information Technology

This project team’s goal was to devise a way for clinicians to consistently identify and document high-risk Medicare patients, so that they can then develop and implement strategies for reducing their risk of rehospitalization. This goal aligns with our participation in CMS’s Value Based Purchasing (VPB) program, which rewards home health care organizations financially for keeping their patient rehospitalization rates low.
The team began by analyzing the existing risk-assessment tool being used. Their analysis revealed an average time lag of three-and-a-half days in delivering the assessment results. They also found the tool was not available for all patients, and that clinicians did not always have access to the risk assessments. In response, the project team developed a new, real-time, evidence-based rehospitalization risk-assessment tool for clinicians, along with a process to ensure that the tool is consistently available and accessible.
When the tool was piloted, the team found it reduced the time required to generate risk assessments from 3.6 days to just .6 days. This enhanced system is enabling clinicians to address their patients’ risk factors more promptly and consistently, resulting in decreased hospitalization rates and improved clinical outcomes, as well as VPB-related financial benefits for the provider.

Home Care and Hospice Care: Standardizing the Monitoring and Treatment of Complex Wounds
Project Leads
- Fortune Grunin, Clinical Account Manager, Business Development
- Gloria DiFeo, Director, Strategic Account Development, Business Development
- Tameka McCabe, Director, Wound Care Management, Quality Care Management
- Xiomara Guerra, Quality Improvement Manager, Quality Care Management

This project team conducted a deep dive into all aspects of clinical wound care in VNS Health’s Home Care and Hospice Care programs. Based on what they found, the team established a standardized approach measuring, monitoring and documenting wounds across VNS Health’s business lines, using a new digital wound monitoring app from Swift Medical.
In addition to giving clinicians an easy way to accurately and consistently monitor and document how patients’ wounds are healing, the app’s related Swift dashboard helps Wound Ostomy and Continence Nurses (WOCN) proactively identify patients who require wound consults and make treatment recommendations. This project has led to substantial changes to how wound care is managed throughout the organization, resulting in improved patient outcomes, faster response for wound consults, and increased transparency about which wounds are healing and which are stalled.

Behavioral Health: Improving the Health Home Program’s Operations
Project Leads
- Marlene Louissaint, Procurement Manager, Procurement and Contract Management
- Sandy Merlino, Vice President, Business Development
- Esmeralda Kila-Lapa, Data Reporting Analyst, Quality Care Management
- Suzette Toussaint, Quality Improvement Manager, Behavioral Health
- Vipul Khamar, Director, Business Systems, Information Technology

In this project, the team focused on improving the clinical processes and workflows in the Behavioral Health team’s Health Home program. These improvements are directly impacting quality of care and facilitating an increase in the Health Home program’s capacity, resulting in improved revenue from insurance reimbursements for care provided.
The team’s initial analysis phase identified numerous problems in how the program planned for, implemented and documented encounters with current or potential clients. Steps taken to address these issues included streamlining the assignment of Health Home cases to care managers, revising policies around how encounter with client are managed and documented, scheduling face-to-face encounters (which are reimbursed at a higher rate) earlier in the month, and following up later in the month with clients who turned down opportunities for a face-to-face encounter, and coordinating more closely to hospitals to gain access to clients who are hospitalized.
These important changes led to an increase in meaningful encounters and timely services for clients, and a related reduction in non-meaningful engagement activities for the client and the Health Home team members.The project also Increased the percentage of clients who meet the program’s required number of client contacts per month from 42% in January 2022 to 72% in August 2022.

Hospice Care: Reducing Hospitalizations of Hospice Patients
Project Leads
- Sadi Benzaquen, Director, Hospice and Palliative Care Outreach, Hospice Care
- Lauren Dauro, Data and Reporting Analyst, Hospice Quality Care Management
- Suzana Celojevic, Quality Improvement Manager, Quality Care Management
- Cheryl Tang, Associate Director, Membership Eligibility and Analytics, MSO
- Oliver Morales, Quality Improvement Manager, Hospice Quality Care Management

This project explored and identified potential solutions for reducing the CMS measure of Burdensome Transitions Type I—representing the percentage of hospice patients who are discharged from hospice care and subsequently admitted to a hospital within two days of being discharge, and then are readmitted to hospice within two days of their hospital discharge. This situation typically occurs when a patient’s symptoms are not being managed effectively in their home hospice setting, leading the family to seek out hospitalization in order to stabilize their loved one’s symptoms before returning to hospice care. Such episodes result in substantial medical costs and also have a negative impact on the patient, their family and the hospice team.
The project team began by focusing on the specific elements involved in patients being discharge from hospice. For example, the team found that even though these hospice patients typically had a home clinician visit within the three days prior to being discharged from hospice, 55% of those patients still went to the hospital following discharge. Further analysis identified that of the patients who were discharged from hospice, 39% had a diagnosis of neoplasm, 29.9% had a cardiac diagnosis, and 30.8% had a nervous system diagnosis. The team determined that by focusing on these common diagnoses, hospice clinicians can more easily identify patients at risk for hospitalization and intervene sooner.
Other recommendations included enhanced training in symptom management and document for this at-risk group, better education of family members, and a heightened focus on managing the care of patients who are admitted on a more frequent basis. The team will continue to work on reducing this important CMS metric going forward.