“Now That’s Teamwork!”: How Three Live-In HHAs and Their HHA Supervisor Care for Their Client—and Each Other
Introducing Now That’s Teamwork—a new Frontline series that features VNS Health teamwork in action.


When home health aides Yolanda Campbell, Jennifer Moulton, and Judith White originally started caring for Sebastian Greene*, they were primarily tending to his wife, who had dementia. When her condition worsened and 24-hour care became necessary, the team transitioned to a live-in situation. Then when Mrs. Greene was ultimately hospitalized, the decision was made to keep the same team, on a live-in basis, for Sebastian, who is in his 90s. Sebastian’s wife died shortly after that, so she never returned home.

“It was a difficult time for Sebastian—they had been married for over 65 years,” says Yolanda. “It’s still an open wound, but things have gotten much better for him now. I know that having the same team of home health aides is a comfort to him.”
A tight schedule—and a tight-knit team
Because of Sebastian’s complex medical needs, it’s critical that somebody always be there with him. Yolanda works from Sunday through Tuesday, Jennifer from Wednesday through Friday, and Judith on Saturdays. All shifts begin (and turn over) at 9 a.m.

“Reliability, attentiveness, and patience are extra important in a live-in situation,” says Deloris Collins, HHA Supervisor with the Queens Unit. “This team not only knows the client well, but they’re extremely punctual, diligent, and work together well. When they do need time off, they let me know far in advance. They never call out in the last minute, leaving me scrambling to find someone to fill in. I supervise up to 100 HHAs at any given time, and I am used to emergencies and schedule changes, but this is a team that I don’t have to worry about. They make my job easy!”
Around-the-clock vigilance

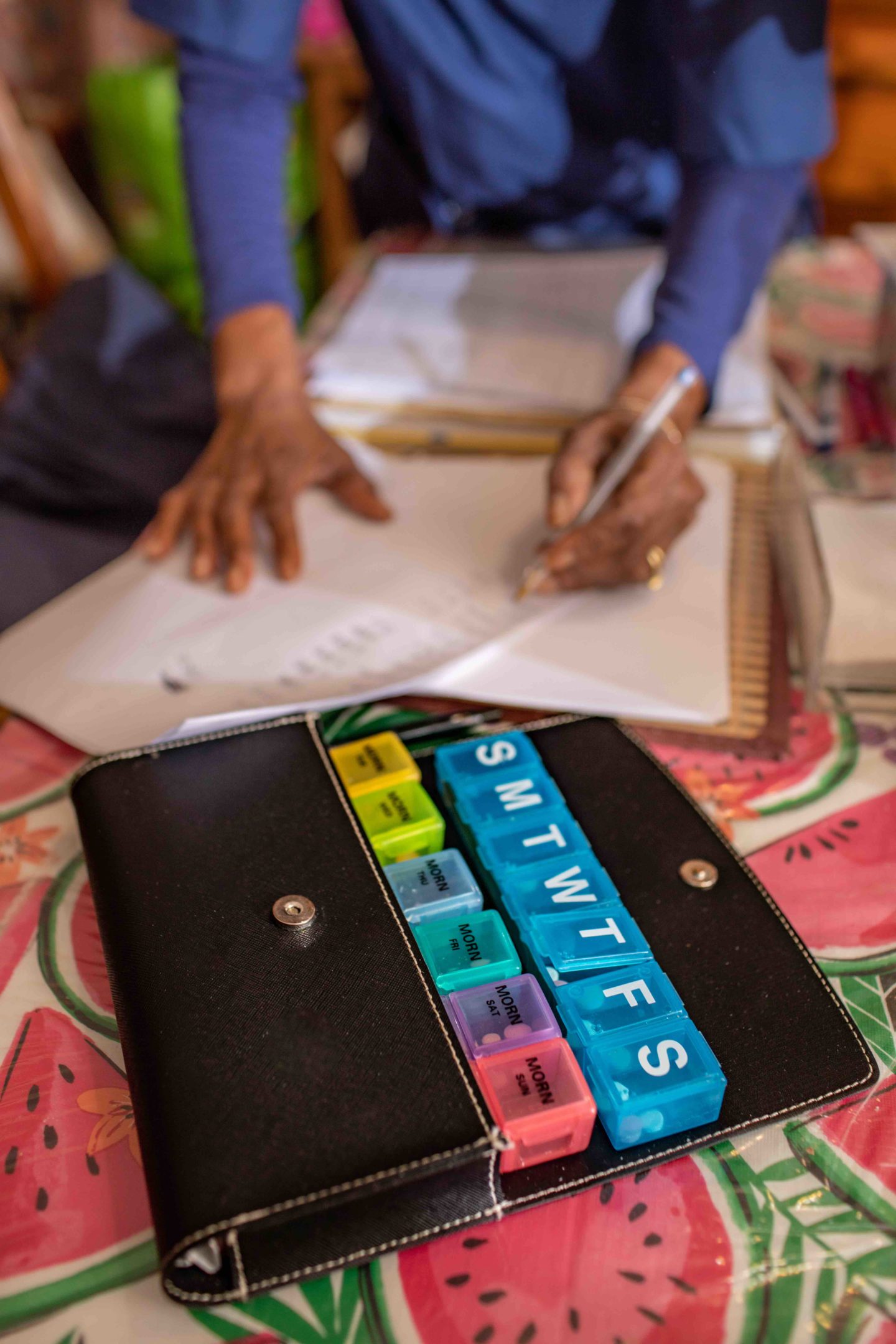
Like most patients who require live-in aides, Sebastian has intricate medical needs, including hypertension and edema. “First thing in the morning we take his blood pressure, weight, oxygen levels and temperature, then we wash him up and make breakfast,” says Jennifer. “He has foot and skin issues as well, so we apply special creams and lotions to his body. He takes his medications at specific times throughout the day, and we have to make sure he not only puts the meds in his mouth but swallows them.”
Because of his edema, Sebastian also has to wear compression boots, keep his leg elevated, and limit his water intake—another thing his team is on top of. “He doesn’t have dementia, but he does get distracted, so it’s vital that we remain aware and attentive at all times,” notes Yolanda.
Communication and collaboration
After more than a year of working with their client and each other, the trio and their supervisor function like a well-oiled machine. In addition to sharing in Sebastian’s medical care, chores like laundry duty are handled fairly and are tackled in turns by the live-in aides. “Working together is key,” says Jennifer. “If something happens during our shift, we always give a detailed report to the next aide when she comes in.”
“We know that we can always count on each other,” adds Judith. “We all want the best for our patient.”
Because of the complexities of Sebastian’s care, whenever there is a scheduling emergency—or even a scheduled absence—the team goes the extra mile to cover all bases. “We’ve had some wonderful fill-in aides, but not all of them have been up to the task,” says Yolanda. “You really need somebody who’s had experience with complicated cases like this. When somebody new comes in, I always make sure that they come in early so I can fully explain the situation. I also check in on them later, and ask them to call me with any questions they might have.”
The challenges and rewards of living in
With their children grown and with their families’ blessings, Yolanda, Jennifer and Judith are happy with their live-in arrangement. “Getting a good night’s sleep was a bit tough when Mrs. Greene was at home,” says Yolanda. “Due to her dementia, she would often call out for us throughout the night—we sleep downstairs, but we have a room monitor. Sleep isn’t as much of an issue anymore, though of course we have to stay vigilant and alert.”

The three all agree that the plus side of living in is an increased connection with their client. “Sebastian is like a family member now—he looks forward to seeing each of us in the morning, and when one of us leaves at the end of our shift, he tells us that he’s going to miss us,” says Jennifer. “When he’s hot, he wants to make sure we’re not too hot. And when he’s cold, he wants to make sure we’re warm. He cares, and that’s what makes it all worthwhile.”
* The patient’s name has been changed for privacy.


