VNSNY Introduces LGBTQ+ Care Type: A New Care Delivery Model Tailored to LGBTQ+ Patients, Clients and Members
VNSNY has long been a leader in providing safe, whole-person, culturally sensitive care to all LGBTQ+ individuals. The organization is now taking this approach to the next level with the introduction this month of the LGBTQ+ Care Type care delivery model—an important step that is especially fitting during Pride Month!
The “Care Type” model takes into account specific aspects of a person’s health profile. In this case, it references patients, clients and plan members who self-identified as LGBTQ+ at a referring organization and who, upon intake to VNSNY, or at any time during their care, elect to take advantage of VNSNY’s LGBTQ+ program or services.
Important elements of the organization-wide program include staff training and awareness, data collection to inform and improve outcomes, and a highly collaborative and integrative approach to ensure 360-degree, inclusive care for all patients. For example, the Care Type model can help determine which health screenings and health education will best serve an LGBTQ+ patient, client or member.
 This new initiative builds on VNSNY’s commitment to provide SAGECare training to employees in every part of our organization, including education on LGBTQ+ cultural issues and best practices around sexual orientation and gender identity.
This new initiative builds on VNSNY’s commitment to provide SAGECare training to employees in every part of our organization, including education on LGBTQ+ cultural issues and best practices around sexual orientation and gender identity.
“Our goal is to provide the highest quality of care and wellness for New York’s LGBTQ+ population,” says Arthur Fitting, VNSNY’s LGBTQ+ Program Manager. Use of the Care Type will not only help to identify LGBTQ+ patients’ medical needs, notes Arthur, it will also help in evaluating patients’ support systems and linking them to LGBTQ+ community resources.
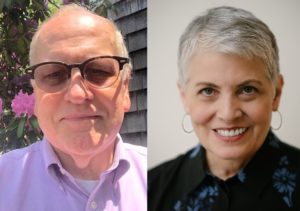 To mark the program’s implementation, Arthur recently spoke with Dr. Barbara Warren, who directs LGBT Programs and Policies in the Office for Diversity and Inclusion at the Mount Sinai Health System, and who is a global leader in LGBTQ+ health equity and advocacy. Below is an excerpt of their conversation.
To mark the program’s implementation, Arthur recently spoke with Dr. Barbara Warren, who directs LGBT Programs and Policies in the Office for Diversity and Inclusion at the Mount Sinai Health System, and who is a global leader in LGBTQ+ health equity and advocacy. Below is an excerpt of their conversation.
Arthur Fitting: At Mount Sinai, you are leaders in advancing care and access for the LGBTQ+ community. As VNSNY launches this new Care Type—the first of its kind in home care, we believe—can you talk about how it can help elevate care for LGBTQ+ New Yorkers?
Barbara Warren: There are lots of dots that intersect in terms of finding out how people identify themselves and how that may contribute to their experience of health care, including home care. Sexual orientation and gender identity are sometimes relevant to the direct care that’s happening and sometimes not—but they are always relevant to patients’ lives. We want people to feel like they don’t have to hold anything back, and that they can present their full selves and their lived experience in the context of their health care. We’ve got to normalize it, just like we ask people about all kinds of other things in order to treat them most effectively for a health condition. Being open, trusting and fully present is healing in itself.
We all have unconscious biases. It’s protective, it’s primal. When we talk in the context of our biases about sexual orientation and gender identity, it can work in both directions, and
people are often surprised that their unconscious biases might affect their caregiving or their decision making. That’s an important focus…that causation of some of the issues in healthcare and health disparities is systemic. We have to be looking at how we might be perpetuating that systemically in our system.
AF: The Care Type will also help us collect data—though only when patients self-identify, I want to emphasize—to better inform the care we deliver and to lead the way for other home- and community-based care organizations. Can you talk about the importance of data in driving outcomes and driving change?
BW: It’s important for those of us doing this work to be able to demonstrate our outcomes and demonstrate how powerful and positive they are—for ourselves and for our patients. VNSNY has been doing the work. You’ve been leading the way in home care, and you’ve been doing it well. Take for example your program that provides specialized care after gender affirmation surgery. I have to say, Wow. That was the first in the country—nobody else was doing anything like that in a visiting nurse capacity.
You know you’re doing the right thing, and you know anecdotally that your patients are benefiting, both in terms of their health status and their patient experience. As a national model, you’ve got to be able to back that up. So now you will be collecting the data, locating where the issues might be, and demonstrating your success in solving them. It’s about doing the right thing, and it’s also about the science and the data.
AF: We are rolling out the Care Type across our organization and training all staff members in what it is, how it supports the patient, and how my role will help to support the staff. What’s the importance of integrating this level of support throughout a large organization, and what are the challenges?
BW: At Mount Sinai, we’ve now been able to track and audit around 30,000 queer-identified people who are coming in every door of our system, so every part of Mount Sinai needs to be queer-inclusive. We’ve been focused on integrating sexual inclusion and gender identity concerns into all the clinical and other education that we do, so it’s not a separate thing. It’s really important to make sure that the education is there at any door the patient walks through.
This is really important for VNSNY too, to educate your health care workers so that with any door they walk through—as opposed to the patient walking through the door—they are prepared to deliver inclusive care. When you’re attending to a patient who just had a hip replacement, for instance, whether they’re gay or straight or trans may have no relevance to their medical post-surgical status. But where it does have relevance is that you’re in a person’s home, and they don’t have to withhold who they are. Withholding identity adds a layer of stress on top of the stress they’re already experiencing with their medical condition.
AF: We are committed to being an organization where New York City’s 780,000 LGBTQ+ residents can trust that they will receive excellent, safe and compassionate care anywhere along the continuum. In your organizational training, you’ve taught staff members how vital that first point of connection is with a patient. How can VNSNY’s LGBTQ+ Care Type help ensure that patients know they are safe and welcome from the first point of entry?
BW: What we’ve done is to work on the front lines, dialoguing with employees, not just mandating. That’s a good model. We have a training for security guards, for example, on creating a welcoming environment. I asked them, ‘What do you think about this? What kinds of tools and resources do you need? Why does it matter to you?’ We worked with staff people from the perspective of experience-based co-design, which is something that can be really helpful—not just top down, but bottom up.
AF: Mount Sinai has been at this for a long time. At VNSNY, we’ve been making steady progress, achieving platinum status with our SAGECare training a few years ago, and we demonstrate our commitment to the LGBTQ+ community every day. As we take this great step forward with the Care Type, what words of encouragement do you have for us?
BW: Know that the work is ongoing. The number one thing we have is complete and utter devotion from leadership to giving us the tools and the resources and the staff that we need. We have a fairly large office for Diversity and Inclusion at Mount Sinai, but you don’t really need a large office. What you need is a champion in leadership who is committed to inclusion, and who makes things available.
AF: That’s great to hear, and we continue to work closely with our leadership here at VNSNY, as well.
BW: It’s hard work to shift the system, both for the staff and the people you serve. It takes all hands on deck, and programs like yours, in collaboration with programs like Mount Sinai’s, magnify the impact we can have on the LBGTQ+ community. This work is so important. Queer people are coming forward. They’re paving the way for the future generation, for young people who are queer to know that the health systems they’re entering will be safe, compassionate and competent.
AF: I’ve been so inspired by the truly groundbreaking work that you’ve done at Mount Sinai over the years and by the impact your work is having on the LGBTQ+ community, the healthcare systems and health education—however everyone benefits when you raise the standards for accessible, inclusive, high quality care. As a member of the LGBTQ+ community and a health care professional, I just want to thank you so much for sharing your insights, experiences and encouragement—as we set what I firmly believe is a bold new precedent for home care: to meet people where they are and treat them as their authentic selves. That is, after all, what high-quality home health care is all about.

